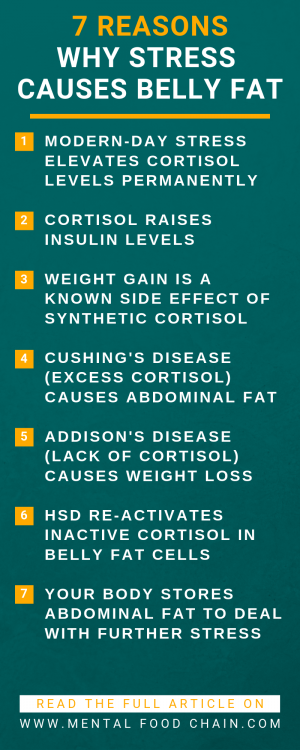
Evidence shows that stress causes weight gain without overeating through the relationship between insulin and cortisol. Learn what you can do to counteract this mechanism.
Cortisol mobilizes energy to deal with stressors through the fight or flight response. Subsequently, blood glucose triggers insulin release.
As your body’s storage hormone, insulin promotes fat storage, drives obesity, and will inhibit your weight loss ambitions.
Learn how the relationship between insulin and cortisol affects your body.
Therefore, this article helps you to understand how chronic stress causes weight gain through persistently high cortisol levels.
Stress and Weight Gain: Cortisol
The adrenal glands secrete cortisol in response to stress. Hence, cortisol is your body’s primary stress hormone.
You might also know cortisol as synthetic cortisone or hydrocortisone. The body needs cortisol to maintain standard psychological processes during stressful situations.
Consequently, the steroid hormone is crucial for effective stress response.
The human body has a default set of physiological reactions to threats called the fight or flight response.
Cortisol is vital to get the body ready for action – to fight or flee. Therefore, nature designed our bodies for acute, not chronic stress (Talbott 2007).
In paleolithic times, that meant scenarios crucial for survival, like a bear charging up your way. After cortisol is released, it immediately enhances glucose availability (Owen and Cahill 1973).
The mobilized energy is aiming at powering muscles and eventually be able to flee and survive.
Furthermore, the induced focus on the body’s survival mechanism limits vital long-term metabolic functions like digestion and growth.
In a process called gluconeogenesis, proteins are broken down and converted into readily available blood glucose. Moreover, cortisol can even stimulate amino acid breakdown from skeletal muscle mass.
It either is directly consumed by muscles or converted to glucose by the liver. Besides insulin, cortisol is a significant player in glucose metabolism.
Because mobilized glucose is burned off to flee from the stressor or fight it.

After mastering the situation, either blood glucose and cortisol levels dropped back to normal, or our paleolithic ancestors were dead.
Hence, adaptive stress responses are a healthy and vital thing. But there is a caveat. Modern-day stressors are difficult to fight off or flee from. Thus they don’t promote acute but chronic stress (Fung 2016).
Stress and Weight Gain Without Overeating
Cortisol is a steroid hormone that makes stored energy readily available.
Insulin, on the other hand, is a storage hormone.
Especially at mealtimes, the body’s insulin levels are high and promote the storage of energy as fat and glycogen.
Based on acute, not chronic stress, insulin and cortisol play opposite roles. And that’s also how nature designed them to function.
But what is chronic stress?
As we know, modern life offers recurring, long-term psychological stress. For example, in the form of mortgage payments, traffic jams, credit card bills, or project deadlines.
Usually, there is no way to run away from chronic stress and burn the energy mobilized by cortisol. Hence, blood glucose and cortisol levels stay elevated.
Furthermore, there is no resolution to the stressor. In light of chronic stress, cortisol and insulin can have similar weight gain effects. Consequently, stress and weight gain are linked.

How Stress Causes Weight Gain
Due to psychological stress, blood glucose levels can stay high for months, which triggers the secretion of insulin from the pancreas.
In short, chronically elevated cortisol levels cause high insulin levels, which promote energy storage and eventually stress-induced weight gain.
The storage hormone insulin is known as the primary driver of obesity. Accordingly, about 75% of weight loss response in obesity and weight regain can be predicted by insulin levels (Kong and Wuillemin et al. 2013).
Swedish researchers observed that increase in self-perceived stress results in elevated cortisol levels and additionally elevates blood sugar and insulin levels.
According to the stress and weight gain study, psychological stress increases body mass index and causes abdominal obesity with metabolic abnormalities (Rosmond and Dallmann et al. 1998).
Based on research, permanently elevated cortisol levels lead to significantly increased insulin levels (Whitworth and Williamson et al. 1994).
That’s a logical outcome since cortisol raises blood sugar while insulin is lowering it.
Cortisol is a glucocorticoid — a steroid produced in the adrenal cortex to raise glucose. Therefore, it can breakdown muscle for glucose mobilization.
Over time chronic stress fosters the development of insulin resistance in liver and muscle cells. In detail, insulin resistance is the body’s impaired ability to process insulin.
Additionally, insulin resistance causes even more insulin production, which leads to increased insulin resistance – a self-enforcing cycle and an enormous driver of obesity.
Accordingly, research obtained lots of evidence for cause and effect characteristics of the cortisol and insulin relationship. And this is how stress causes weight gain (Rizza and Mandarino et al. 1982).
Stress and Weight Gain Studies
There is a straightforward way to verify if high cortisol levels and hence stress can make you fat.
Luckily, cortisol’s synthetic brother, prednisone, can induce consistently elevated cortisol levels. And according to research, it causes weight gain. Moreover, weight gain is the most common side effect of prednisone.
Therefore, long-term chronic stress causes weight gain (Fung 2016).
Furthermore, studies confirm that long-term use of prednisone can lead to insulin resistance and even full-blown diabetes (Jindal 1994).

Comparatively, let’s take a look at Cushing’s disease studies. Cushing’s syndrome is a disease mainly characterized by consistent excessively high cortisol secretion.
Besides a very high risk of developing diabetes, rapid weight gain is almost universal for Cushing’s disease patients.
According to research, 97 percent of patients suffering from Cushing’s disease experience abdominal fat gain, and 94 percent overall weight gain.
No matter how much people eat or exercise, high cortisol levels and hence stress causes weight gain without overeating (Tauchmanovà and Rossi et al. 2002).
Furthermore, Scottish researchers found that excess cortisol secretion leads to increased waist-to-height-ratio and abdominal fat gain in people without Cushing’s disease.
That’s especially alarming since belly fat more intensively contributes to health issues than overall fat gain (Fraser and Ingram et al. 1999).
Stress and Weight Loss Studies
If high cortisol levels are causal for weight gain, can lowering cortisol levels induce weight loss?
Glad you asked. Addison’s disease is the opposite of Cushing’s syndrome when it comes to body weight.
Therefore, its most common side effect is weight loss. Addison’s disease is adrenal insufficiency. Due to a damaged adrenal gland, cortisol levels are low.
The primary symptom of Addison’s disease is weight loss. Accordingly, about 97 percent of people who have Addison’s disease experience weight loss due to low cortisol levels (Fung 2016).
Similarly, prednisone (synthetic cortisol) withdrawal from patients caused a significant loss in body weight and more interestingly abdominal fat (Lemieux and Houde et al. 2002).
In conclusion, the reverse of the argument that chronic stress can make you fat is correct. Since there is scientific proof, lowering cortisol levels causes weight loss.

Stress and Weight Gain in Stomach
While low cortisol levels help to reduce body fat, high cortisol levels, and hence stress causes belly fat. But the equation isn’t that simple.
There is another factor when it comes to stress and weight gain called 11 beta-hydroxysteroid dehydrogenase-1 (HSD).
HSD is an enzyme found in fat cells that primarily occurs in adipose fat, liver, and brain tissue.
Because of HSD’s functioning within fat cells, it’s als known as our body’s fat storage enzyme.
Moreover, HSD re-activates cortisone – inactive cortisol stored in fat cells. As a result, the activated cortisol stimulates fat storage within the cell (Ayachi and Paulmyer-Lacroix et al. 2006).
This functioning is concerning the critical abdominal fat cells. Researchers found that the fat-storing signal of HSD is more intense in belly fat cells and especially affects type 2 diabetes patients (Dube and Norby et al. 2015).
Therefore, chronic stress can cause belly fat in an alarming and often rapid way. HSD acts like a hidden enemy in your own team. Because even if you’re focusing on lowering stress, HSD can still amplify belly fat gain.

And as a local amplifier, it can force belly fat cells to be exposed to a high amount of cortisol from the inside, no matter if blood cortisol levels are low.
Since it can explain more complex cases, the activity of HSD has been the missing link between stress and weight gain in research.
So far, no lifestyle factors such as exercise or stress are known to impact HSD activity directly. In other words, HSD’s individual impact on weight gain is genetically defined (Talbott 2007).
Lack of Sleep
The simplest and most effective method to lower chronic stress is getting a sufficient amount of sleep.
Although that sounds very logical, we tend to do the exact opposite. One century ago, people used to sleep for approximately nine hours. But sleep duration has been declining steadily.
As a result, almost a third of working adults are getting less than six hours of sleep per night today (Webb and Agnew 2013).
Based on a meta-analysis of short sleep duration and obesity as much as five to six hours of sleep are associated with a 50 percent increased risk of weight gain (Cappuccio and Taggart et al. 2008).
Furthermore, sleep deprivation stimulates cortisol leading to high insulin levels and insulin resistance. Hence, as little as a single night of sleep, deprivation doubles cortisol levels (Joo and Yoon et al. 2012).
Furthermore, lack of sleep can affect the resiliency of the fight or flight response. According to research, sleep loss results in a delayed elevation of cortisol levels.
Effects are taking place next evening and are also impacting metabolism (Leproult and Copinschi et al. 1997).
Dealing with Stress and Weight Gain
With this in mind, adequate sleep is the most effective method for stress reduction.
According to studies, the ideal sleep duration is 8 hours and 15 minutes, with 7 to 9 hours being the healthy range.
Therefore, deep sleep for just one or two nights can lower cortisol levels more than years of stress management classes (Talbott 2007).
Also, sleep helps with mood swings, anxiety, and depression. In addition, sleep improves energy levels and metabolism.
Nevertheless, dealing with stress and weight gain is not limited to getting more sleep.
Researchers at the Alberta Cancer Board have shown that gentle activities like meditation, yoga, and relaxation exercises are quite impactful.
Their mindfulness-based stress reduction (MBSR) approach decreased stress symptoms while increasing sleep and overall quality of life of cancer patients (Carlson and Speca et al. 2004).
And to get deeper insights into how yoga, meditation, and other methods can reduce chronic stress, I recommend using my simple but effective stress management techniques PDF List.
You might be surprised how easy it is to start fighting chronic stress today.
Conclusion
Stress can cause weight gain without overeating through the relationship of insulin and cortisol. While the stress hormone cortisol raises blood sugar levels, the storage hormone insulin lowers them.
On the contrary to short-term acute stress, chronic stress can lead from these opposing roles of cortisol and insulin to similar weight gain effects.
Due to persistent psychological stress, cortisol steadily mobilizes energy, which insulin stores as fat.
Hence, chronic stress causes weight gain and promotes insulin resistance – the primary driver of obesity.
Moreover, the enzyme HSD can further amplify stress-induced weight gain by re-activating cortisol inside belly-fat cells.
Frequently Asked Questions (FAQ)
Can stress cause you to gain weight?
Yes, because the primary stress hormone cortisol raises levels of the storage hormone insulin, which eventually causes weight gain.
Can stress keep you from losing weight?
Yes, stress can keep you from losing weight. Since the stress hormone cortisol mobilizes energy in the form of blood glucose, your body releases insulin. The storage hormone insulin inhibits weight loss.
Can stress hormones cause weight gain?
Yes, because you can’t run away from chronic stress, it keeps cortisol levels high. The primary stress hormone cortisol mobilizes energy in the form of glucose. High blood glucose triggers the secretion of the primary (fat) storage hormone insulin. As a result of the persistent stress hormone secretion, high levels of insulin are causing weight gain.
What is a stress belly?
A stress belly is the human body’s response to chronic stress. To be prepared for future stressors, the body preferably stores energy in the abdominal region as belly fat near the liver, where it’s readily available.
References
A – E
F – O
Fung J. The Obesity Code: Unlocking the Secrets of Weight Loss. Vancouver: Greystone Books, 2016.
P – Z
Mag. Stephan Lederer, MSc. is an author and blogger from Austria who writes in-depth content about health and nutrition. His book series on Interval Fasting landed #1 on the bestseller list in the German Amazon marketplace in 15 categories.
Stephan is a true man of science, having earned multiple diplomas and master's degrees in various fields. He has made it his mission to bridge the gap between conventional wisdom and scientific knowledge. He precisely reviews the content and sources of this blog for currency and accuracy.
Click on the links above to visit his author and about me pages.